Decoding Cannabis: Medical cannabis for fibromyalgia, a real-world study review
17 min read
Sam North
Medical cannabis may not be a cure for fibromyalgia, but for many UK patients, it’s helping reduce pain, improve sleep, and ease reliance on conventional meds. This real-world study shows how cannabis could reshape chronic pain treatment.
Contents
Fibromyalgia is notoriously difficult to manage. It’s not just chronic pain that the condition causes - it’s the fatigue, disrupted sleep, mental fog and emotional strain that all make up a fibromyalgia sufferer’s day-to-day life. These secondary effects can be just as debilitating as the pain itself.
Pharmaceuticals, lifestyle changes and holistic therapy options can (and in some cases really do) help to a degree, but for many people battling fibromyalgia, the results are inconsistent. Treatment becomes a cycle of trial and error, where side effects from the heavy painkillers prescribed are all too common, and true progress towards a pain-free life is slow.
In this instalment of Decoding Cannabis (our series where we unpack one key research paper on medical cannabis treatment and translate the findings into plain English), we’re turning to a 2019 real-world study titled “Safety and Efficacy of Medical Cannabis in Fibromyalgia.”
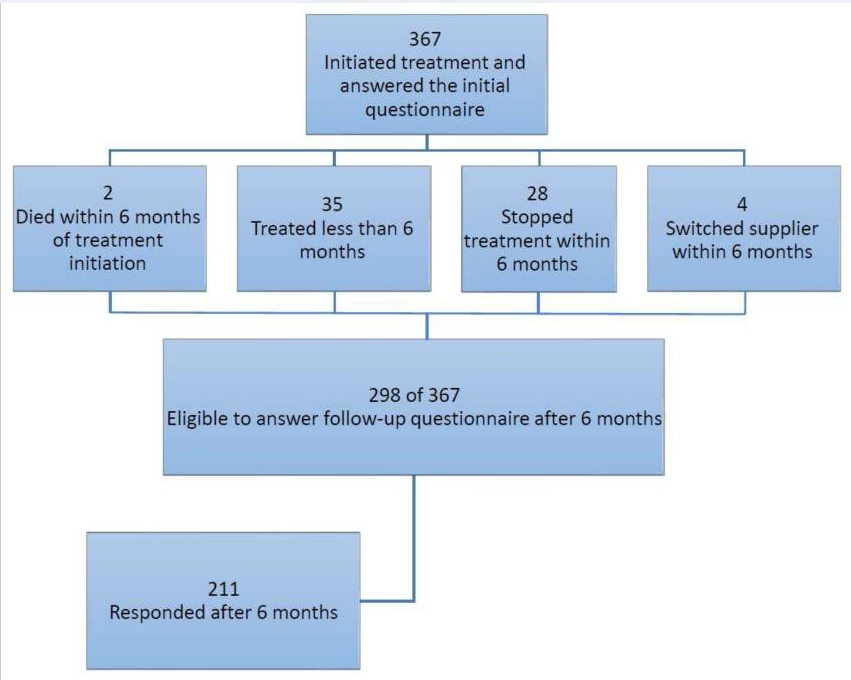
The researchers followed 367 people through Israel’s national cannabis programme, all living with fibromyalgia and struggling with symptoms that had resisted standard care.
What they found went far beyond just pain relief.
What is fibromyalgia, and why are current treatments often ineffective?
Fibromyalgia isn’t a new disease. People suffering from the main group of fibromyalgia symptoms have been described in medical texts as early as the 1800s, but it wasn’t until 1976 that the term “Fibromyalgia” first appeared, and it wasn't until the early 1990s that it was formally recognised as a real, diagnosable condition.
And even now, the mechanisms behind the condition are still not fully understood.
What sets it apart isn’t just the chronic pain, but the collection of secondary symptoms that have historically made it such a difficult condition to categorise:
- Cognitive problems: Concentration, memory, and analytical thinking can all be affected, often described by patients and medical professionals as “fibro fog”
- Sleep issues: Trouble falling asleep, staying asleep, or getting deep, restorative rest is common
- Emotional distress: Ongoing fatigue and pain can lead to anxiety, low mood, and, in some cases, depression
- Physical exhaustion: Even small tasks can feel draining, with energy levels that crash unpredictably, and when they do, the pain and other symptoms often increase.
- Sensory sensitivity: Some people experience increased sensitivity to noise, light, touch or temperature
- Muscle stiffness: Many experience persistent tightness or aching, particularly in the morning
- Headaches and dizziness: Migraine-like headaches and spells of light-headedness are often reported
- Vision changes: Blurred or strained vision can flare up, especially during periods of fatigue
While medical cannabis isn't a cure and can’t treat every one of these symptoms, it does offer patients the potential to manage several at once, particularly chronic pain, sleep disruption, mental health concerns, and more.
And for many, that’s enough to make everyday life feel possible again.
Why is it so hard to treat fibromyalgia effectively?
We still do not fully understand the cause (or causes) of fibromyalgia, and no single or straightforward test to confirm it. That alone makes treatment difficult.
But more than that, the condition affects multiple systems in the body at once, from the nervous system to sleep regulation and mental health. It’s complex, can present as so many other health issues (which makes diagnosis a minefield), and the way that the symptoms appear/affect sufferers is deeply individual.
Standard, conventional treatment plans for fibromyalgia involve a combination of medications and non-drug approaches. These include antidepressants, anticonvulsants, physiotherapy, psychotherapy, and in many cases, opioids.
While they can help reduce certain symptoms, they don’t address the condition in full. The well-documented side effects from the heavy pharmaceuticals often prescribed (including weight gain, drowsiness, digestive issues and dependency) can be really hard to manage.
Even non-drug approaches like physiotherapy and CBT can have limited success when fatigue and pain levels are high. And because fibromyalgia doesn’t look the same from one person to the next, a treatment that works for one patient might do very little for another.
This leaves many people stuck in a cycle of patchy relief, new prescriptions, and the slow grind of trying to piece together something that feels remotely manageable. It’s no surprise that patients desperate for long-term relief have started to look outside the conventional route, which is why interest in medical cannabis for fibromyalgia is beginning to grow.
What did this real-world study on medical cannabis for fibromyalgia aim to find?
In 2019, a group of researchers in Israel set out to answer a long-held question:
“Can medical cannabis actually offer a safe and effective treatment option for people living with fibromyalgia, one that helps with more than just pain relief?”
Their findings were published in the Journal of Clinical Medicine, and the study has since become one of the most widely referenced real-world investigations into cannabis for fibromyalgia.
A closer look at the study design
This study is classed as a prospective observational study. While the researchers themselves didn't assign treatments, patients were receiving cannabis through Israel’s regulated medical programme.
Each person had a prescription, was supported by nurses, and had access to guidance throughout the titration process. The study observed what happened in this real-world clinical setting, without changing or controlling how treatment was delivered.
The aim was to assess both the safety and the effectiveness of medical cannabis in this patient group, with a focus on pain levels, quality of life, medication use, and any side effects during treatment.
Who took part in the study, and how was medical cannabis applied?
The study followed 367 patients over a six-month period. All were part of Israel’s national medical cannabis programme and received treatment through Tikun Olam, the largest medical cannabis provider in Israel (one third of all medical cannabis patients in Israel are patients with this clinic). Every participant had been diagnosed with fibromyalgia and had found limited success with previous treatments.
The average participant was 52.9 years old, and 82% were women, reflecting the condition’s higher prevalence among women. Every patient had been living with fibromyalgia for over a year and had tried other treatment options without success. In short, this was a group of people for whom standard care hadn’t worked.
Click image to enlarge
Cannabis strains and cannabinoid profiles offered in the study
One of the key features of this real-world study was that patients weren’t limited to one product or a fixed dose. Instead, they had access to a range of cannabis strains and were supported by clinical staff in adjusting both the type and amount of cannabis over time (much like Releaf patients).
This gradual, personalised approach, known as titration, allowed patients to respond to their symptoms in a way that felt flexible and manageable. By the six-month point, the median THC content being administered was 20%, while the CBD content averaged around 4%.
In other words, most patients in this group were using THC-dominant strains, rather than balanced or CBD-rich products. This aligns with other recent research around the role of THC for pain reduction and help with sleep issues.
The patients took their prescribed medical cannabis flower through either smoking or vaporising, administration methods that allow for rapid onset of effects and easier day-to-day dose adjustment.
Here in the UK, smoking any form of medical cannabis is illegal, but vaporising dried flower is permitted under prescription and remains the most common method of administration. Like the patients in this study, Releaf patients are guided through titration by our world-class clinical team, allowing them to adjust both dose and strain based on symptom response and side effects.
The study didn’t pit specific cultivars against each other, but the overall cannabinoid profiles were considered and pointed to a pretty clear trend - most patients found the most symptomatic relief when they took THC-dominant flower.
That’s not to say the conversation around THC vs CBD for fibromyalgia is redundant, or that all patients will respond best to THC-heavy formulations. In fact, some may benefit more from balanced or CBD-rich options, particularly if anxiety, inflammation, or sensitivity to psychoactive effects are major concerns.
How did medical cannabis affect fibromyalgia symptoms?
Finally, time to really dig our teeth into the findings.
While pain was the main focus, the researchers were interested in measuring far more than just pain scores. They wanted to find out how medical cannabis administration affected the entire spectrum of symptoms that patients with fibromyalgia battle.
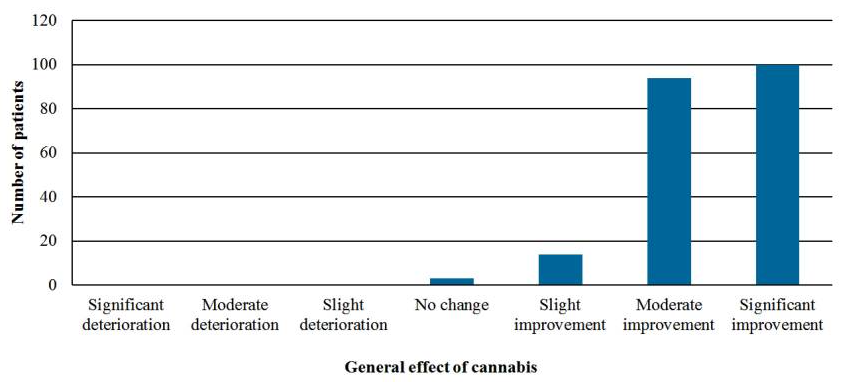
Click image to enlarge
Pain scores improved significantly
This really does show just how strikingly effective medical cannabis can be for chronic pain sufferers. Study participants were asked to self-report their pain scores on a ten-point scale:
- The average pain score fell from nine to five over a six-month period
Pretty compelling results, but this is just the tip of the proverbial iceberg.
Click image to enlarge
Sleep, mood, and daily quality of life improved
Medical cannabis didn’t just reduce pain:
- 86.6% of patients reported better sleep
- 81% reported a reduction in depression
- Some also saw positive changes in appetite and libido, adding to the overall quality of life.
Many patients reduced their use of other medications
Another section of the study that has been backed up by the emerging body of research is that medical cannabis can help patients reduce their intake of heavy pharmaceuticals.
About 22% of participants reduced or stopped using opioids. Another 20% did the same with benzodiazepines. This was a welcome shift away from medications with long-term side effects or dependency risks.
While the study didn’t test cannabis as a direct substitute, it highlights how THC for fibromyalgia and related formulations may offer a route toward fibromyalgia alternative (or complementary) treatments in the UK.
Most side effects were mild and tolerable
While side effects were reported, they were mostly mild and affected fewer than eight percent of participants.
The most common were:
Compared with many of the current treatments offered to people with fibromyalgia, these side effect rates are remarkably low. That won’t mean much to everyone, but for someone who’s spent years juggling prescriptions with sleepiness, weight gain, or brain fog as the trade-off, it matters a great deal.
For UK patients considering medical cannabis, especially those wary of how it might affect daily life, this study offers a quiet reassurance. When introduced carefully, with clinical guidance and room to adjust, cannabis was generally well tolerated.
We aren't shying away from the fact that side effects did occur, but they were infrequent, and mostly mild/manageable.
This doesn’t make cannabis a perfect answer, but it does suggest it could be a gentler one for some, particularly for those who’ve already run the gauntlet of standard care without finding the results they had hoped for.
Who is medical cannabis most effective for in fibromyalgia, and can we trust the results?
Not everyone responded to medical cannabis in the same way. The patients who had prior experience with cannabis saw the best results, along with patients who also experienced spasticity as a fibromyalgia symptom.
On the flip side, patients over the age of 60 and those who came into treatment with concerns or scepticism about medical cannabis efficacy were less likely to see strong improvements.
This suggests that expectations, past exposure, and mindset may all influence how well treatment works - something that echoes other findings in chronic pain care. The stigmatisation of cannabis over the past century seems to still be influencing patient outcomes in subtle but significant ways.
As for the reliability of the results, this was a real-world observational study. That means it was not a randomised controlled trial, and there was no placebo group or blinding. Still, with a large sample size, six-month follow-up, and outcomes that match what many patients and clinicians already report in practice, the findings carry weight.
It may not offer a final answer, but it gives us a clear and credible starting point. And it mirrors what Releaf patients have been sharing with us.
What are UK patients saying about medical cannabis for fibromyalgia?
These aren’t case studies or clinical abstracts - they’re the real words of Releaf patients, shared on our dedicated Patient Stories page.
Each reflects a unique experience with fibromyalgia, and the role that prescribed medical cannabis has played in easing pain, restoring routine, and helping people reconnect with their day-to-day lives.
Rhona
“To be completely honest with you, I was sceptical at best about medical cannabis before I started taking it. I had tried cannabis in the past recreationally, and hadn't associated it with any level of pain relief whatsoever. But, wow! As soon as I started with my prescribed medical cannabis flower through the Omura vaporiser, there was pain relief.”
“I was able to straight away stop using the morphine patches that were my main form of pain relief. I was also able to cut out the sleeping tablets, which was massive for me. I hated the groggy, out-of-it, almost hung-over feeling that I had each morning after taking a sleeping tablet. I would wake up with a headache most days.”
“The very next day, I was able to get back out into the garden. Now I'm back in the kitchen and the garden and loving it! I even mowed the whole lawn a few days ago, and felt great. I haven't been able to do that for years.”

Chaos
“With fibromyalgia, there's actually nothing physically causing the pain - it's the nerve endings which are sending signals to your brain telling you 'You're in pain!' and it just goes on sending these signals for no reason. So, what cannabis does is that it really helps to quiet those nerves down.”
“It really dulls the pain, and it also makes it, so I am not focusing on the pain nearly as much. I used to really struggle with that, focusing on the pain. It was always at the forefront of my mind, and it started to affect my mood quite a bit. I was getting cranky, irritable, and snappy with people because the pain was just so bad.”
“But since starting with medical cannabis, I've been able to get out and enjoy my days again, and I'm finding enjoyment in life again. I'm laughing a lot more. I mean, I'm just having a lot more fun.”

Helen
“Sometimes I was in so much pain that my body couldn’t function. I couldn't even do simple household tasks like cooking or putting the washing on the line.”
“Since I started with medical cannabis, I’ve made incredible progress with my pain, and my agoraphobia is basically gone. I’ve started driving again and doing errands by myself. At first, I was just driving around and coming home, but I eventually found the courage to actually go into town, park my car and go into shops.”
“Physically, there have also been dramatic changes. I've been able to go up and down the stairs again, something else I haven’t done in years... Honestly, you can't beat medical cannabis. I'm a true believer in it.”

Lisa
“My pain levels were extreme. I’d wake up in the morning feeling like an elephant had literally walked up and down my body. Getting out of bed was such a challenge.”
“One of the massive benefits, and one that I wasn’t necessarily expecting, is that I wake up pain-free. I don't have to jump straight into the shower any more just to function. I can start my day like a normal human being.”
“Joining Releaf and starting medical cannabis treatment has been life-changing for me - literally life-changing. So if you're considering it, I would definitely say go for it. You won't know how much it can help until you try.”
Could medical cannabis be part of future fibromyalgia treatment in the UK?
As you can see from the testimonials above, medical cannabis is already changing the lives of UK fibromyalgia patients.
When legally prescribed and clinically supervised, fibromyalgia cannabis treatment is effective, safe, and often far more tolerable than many conventional alternatives. For patients facing constant pain, sleep disruption, and the emotional weight of long-term illness, it offers not just relief, but the chance to re-engage with the things that make life worth living.
Is medical cannabis a cure for fibromyalgia?
No, unfortunately, there is no known cure for fibromyalgia right now.
It remains a complex, somewhat poorly understood condition that affects people in deeply individual ways. But for many, medical cannabis has become an important part of a more manageable, more liveable routine.
It’s not about erasing the condition. It’s about reducing the burden - quietening the symptoms, easing the pain, improving much-needed rest, and boosting the overall quality of life.
If you’re keen to find out more about alternative treatments for fibromyalgia in the UK, and wondering whether this path might be right for you, Releaf is here to help. Head to our fast, free medical cannabis eligibility checker - it takes less than 20 seconds to complete, and you’ll get instant feedback on whether you might be suitable for a legal UK medical cannabis prescription.
Share article
Did you like this article?
It is important to seek medical advice before starting any new treatments. The patient advisors at Releaf are available to provide expert advice and support. Alternatively, click here to book a consultation with one of our specialist doctors.
Elevate your wellness with medical cannabis
Get comprehensive care, convenience, and confidence with an all-in-one treatment plan.
Am I eligible?Authors
Sam North, a seasoned writer with over five years' experience and expertise in medicinal cannabis, brings clarity to complex concepts, focusing on education and informed use.
Editorial Policy
All of our articles are written by medical cannabis experts, guided by strict sourcing guidelines, and reference peer-reviewed studies and credible academic research. Our expert clinical team and compliance specialists provide valuable insights to ensure accuracy when required. Learn more in our editorial policy.
Need more help?