5 common medical cannabis myths and misconceptions debunked
7 min read
Lucy MacKinnon
It has now been almost six years since the legalisation of medical cannabis came into effect in the UK, but still, prevalent misconceptions/myths about these treatments options persist today. Because these are often fuelled by stigmatisations or a lack of knowledge on the subject, we think debunking these common medical cannabis misconceptions can play an important role in improving the current education and awareness of cannabis-based options in the UK. And so, that’s exactly what we’ve done!
Contents
The use and prescription of medical cannabis was legalised in 2018 in the UK, expanding the range of treatment options available for conditions that are often unresponsive to traditional or conventional medicines.
However, as accessibility to cannabis-based options has increased so has the dialogue surrounding them, and the prevalence of the myths and misconceptions that surround medical cannabis, and its usage, have become more clear.
As a medical cannabis clinic, we feel it's our duty to debunk these myths and misconceptions, and improve the education and information available to those who are curious about cannabis-based medicines. So we’ve tackled 5 of the most common medical cannabis myths and misconceptions, so you can make well-informed decisions, and have well-informed discussions.
Myth: Medical cannabis is the same as recreational weed
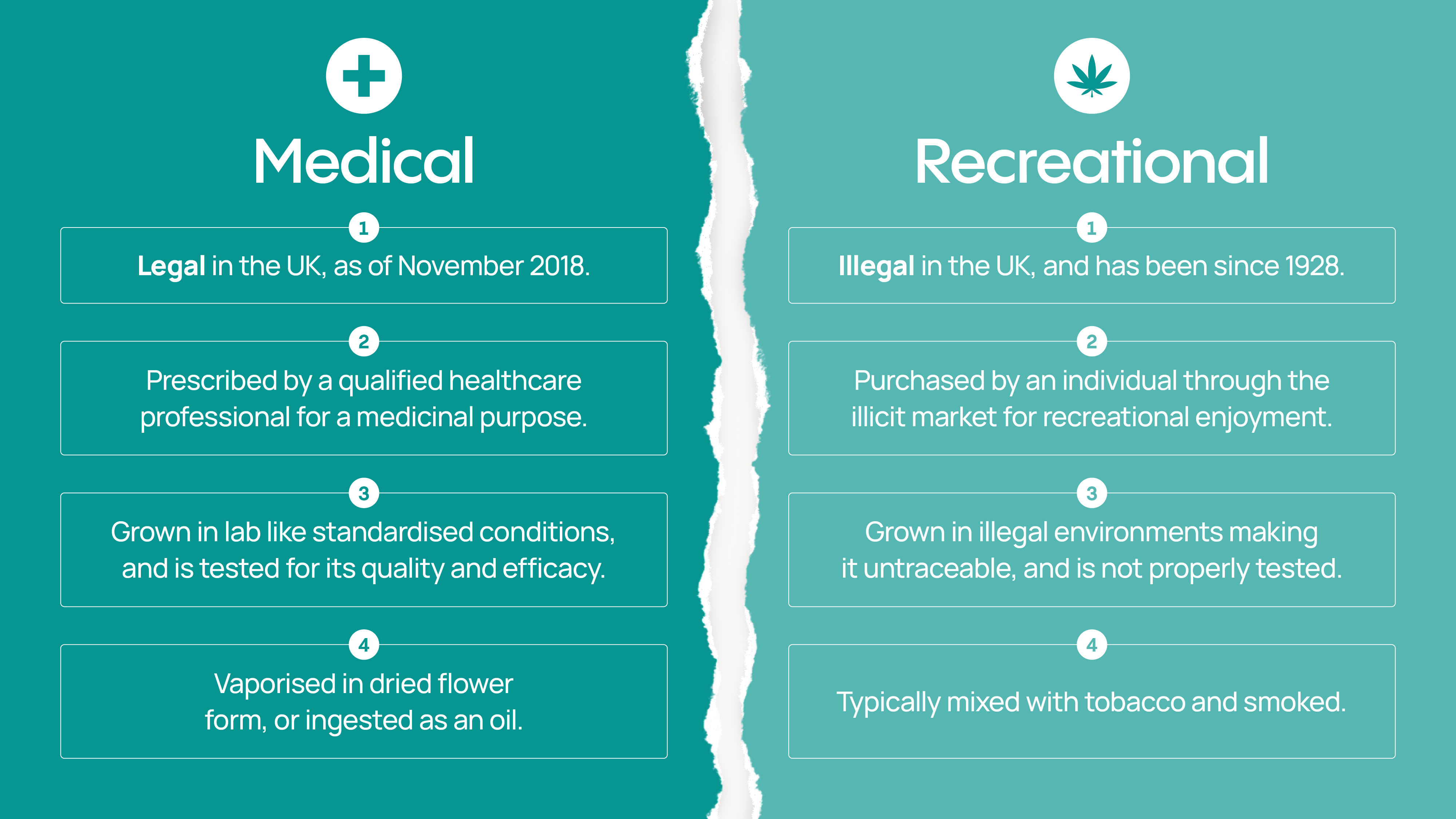
Medical cannabis and recreational weed are both derived from the same plant family (Cannabis Sativa L), and they do share the same chemical compounds and molecular makeup.
But, their legality, the way in which they are accessed, grown, administered, and the purpose for which they are used, are entirely different.
Medical cannabis has been legal in the UK since November 2018, but the use of recreational cannabis remains illegal.
Medical cannabis is strictly used for its therapeutic benefits, is prescribed by qualified healthcare professionals, is dispensed from a legal and legitimate pharmacies, and its application is carefully monitored.
Recreational weed is sourced on the black market - and in the UK, its production, purchase, and possession is a criminal offence. Although there are an estimated 1.8 million people self-medicating with cannabis sourced illegally in the UK, those using recreational weed do so to evoke the euphoric ‘high’ associated with the plant, as opposed to the medicinal benefits it can have for those struggling with chronic conditions.
While recreational cannabis is typically mixed with tobacco and smoked, medical cannabis flower is prescribed to be vaporised, and smoking medical cannabis invalidates its status as a medicine.
To summarise:
Click image to enlarge
Misconception: Medical cannabis is a gateway drug
Cannabis is often called a gateway drug - a statement that implies once a person starts taking cannabis, they are likely to start using ‘harder’ substances or drugs that can be extremely addictive and cause a large range of serious health concerns.
While it is true that taking a cautious approach to using cannabis is advised, the research into whether recreational cannabis is actually a gateway drug remains inconclusive, and it is unfair to reiterate this same sentiment to the medicinal application of cannabis.
In fact, evidence shows that when patients are treated with medical cannabis, often their use of other medications or drugs actually decreases.
This trend has been observed in observational studies in the UK, such as the 2023 MCA patient survey, which found 60% of the patients taking part managed to reduce their intake of prescribed medications after starting a cannabis-based treatment plan.
Similar results have been observed in Australia, Denmark, the US, and Canada. There are also findings to suggest that some cannabinoids could potentially help curb addiction to other substances. Still, research in this area remains limited, and a direct correlation is yet to be established.
Myth: Medical cannabis is a ‘cure all’ treatment.
It is important to emphasise that although medical cannabis can have incredible results for some, it is not a ‘cure all’ treatment, or one-stop solution for any and every medical concern.
While it's true that medical cannabis can take a multifaceted approach in treating a variety of symptoms caused by certain conditions, it is not a suitable option for everyone, or every condition.
Unfortunately, there are people who over-emphasise, overstate, or embellish the effects that medical cannabis can have. While studies show that this plant can greatly improve quality of life for some patients when applied appropriately, making claims such as ‘cannabis cures cancer’ are clinically unfounded and quite simply dangerous.
At times, the lack of side effects associated with cannabis-derived treatments can also lead to the development of ‘wonder drug’ claims, or implications, but these too can be extremely detrimental to the industry as a whole.
While it can be seen through research that medicinal applications of cannabis tend to account for few and minimal side effects - this does not make them a ‘cure’, it just means they were generally well tolerated by the individuals taking them.
Misconception: Medical cannabis isn’t good for mental health
Because of its psychoactive properties, many believe cannabis can be harmful to mental health. Although this may be true for some individuals and medical cannabis will not be recommended for those who have a diagnosis or history of psychosis or schizophrenia, cannabis-based products can be prescribed to benefit a number of mental health conditions.
Certain mental health conditions like anxiety, PTSD, and depression have shown positive responses to cannabis-based treatments during clinical investigations, with improvements noted in not only mood and sleep, but general quality of life, and a patient’s ability to get on with day-to-day activities.
The effects medical cannabis can have on reducing anxiety and stress and promoting relaxation and a calm sense of self can also be extremely beneficial to a wide range of patients with other health conditions and comorbidities.
Often, regardless of what condition is being treated with medical cannabis, improvements in anxiety, mood, and sleep are often noticed soon after starting cannabis-based treatments, and this is regularly mentioned during follow-up appointments with medical cannabis prescribers.
But, it's important to note that medical cannabis treatment plans are carefully monitored by a multidisciplinary team of qualified health care professionals to ensure their safety and efficacy, and medical cannabis should only be used for mental health concerns under professional, expert guidance.
Myth: Medical cannabis is smoked
As we previously mentioned when explaining the differences between medical cannabis and recreational weed, dried medical cannabis flower can be prescribed in the UK to those who may benefit from this treatment option. But, it is always prescribed with the intention of being vaporised - not smoked.
Smoking cannabis, for any reason, remains illegal in the UK. This is because smoking involves combustion, and a number of dangerous and carcinogenic chemicals are released during this process, which can have serious and substantial implications on a person’s long term health.
And, because medical cannabis flowers are prescribed by doctors with the intention of helping their patients' health, not harming it, when cannabis flowers are prescribed, they are done so with the instruction of being used in a vaporiser.
Share article
Did you like this article?
It is important to seek medical advice before starting any new treatments. The patient advisors at Releaf are available to provide expert advice and support. Alternatively, click here to book a consultation with one of our specialist doctors.
Elevate your wellness with medical cannabis
Get comprehensive care, convenience, and confidence with an all-in-one treatment plan.
Am I eligible?Authors
With five years of journalism and healthcare content creation under her belt, Lucy strives to improve medical cannabis awareness and access in the UK by producing high quality, credible content.
compliance checked
Compliance Director
Editorial Policy
All of our articles are written by medical cannabis experts, guided by strict sourcing guidelines, and reference peer-reviewed studies and credible academic research. Our expert clinical team and compliance specialists provide valuable insights to ensure accuracy when required. Learn more in our editorial policy.
Need more help?